14 Jun 2023
Current Unmet Needs in Multiple Endocrine Neoplasia Syndromes
From time to time, AMEND CEO, Jo Grey, is asked to give presentations at conferences and other events, to be the voice of patients with MEN syndromes. What does she tell them and why?
Jo commented that, ‘About half of the time, people, especially medical students, are interested in my personal story of diagnosis, survival and life with MEN2A, but the rest of the time, wider perspectives are required. This is where all those AMEND surveys come in!’
Those wider perspectives usually include evidence of unmet needs for our patient communities. Jo presented on these at the 2022 British Endocrine Society Meeting Nurses’ Session, and at the World MEN meeting in Marseille in April 2023.
What follows here is a summary of those shared perspectives.
-

-
When we describe patient experiences, we are often thinking about the ‘rollercoaster period’ of tests, scans and treatments, as well as the diagnosis of other members who then undergo the same.
Yes, this is a significant part of life with an MEN syndrome; however, first, people need to have a diagnosis.
-

-
The fact is that getting anywhere near to the rollercoaster often means travelling in a long ‘queue’.
In Europe, the average time to diagnosis from onset of symptoms is 5 1/2 years!
This statistic came from a large European survey by the European MEN Alliance, of which AMEND is a founding member (Drewit K P et al, 2021, Endocrine).
There were variations to this statistic: the time to diagnosis was just under 3 years for those diagnosed with MEN2. In addition, and somewhat surprisingly, it took just over 3 years for those with an existing diagnosis in the family to be diagnosed themselves.
-
-
As patients, we often know that this constant waiting and battling for a diagnosis can have an impact on prognosis, and also on emotional wellbeing.
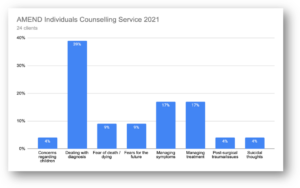
Each year, our Counselling Service provider, Rareminds, produces a report that anonymously shares with us the main issues and themes experienced by people using the service.
You can clearly see from this graph from 2021 (n=24), that most of those contacting the Counselling Service felt that diagnosis (either getting diagnosed or dealing with the diagnosis) was the greatest challenge that they had faced. This trend is repeated every year.
It is most certainly not an issue that should be ignored, and that is why we, together with Rareminds CEO, Kym Winter, developed the leaflet about Dealing with Diagnosis. More work in this area needs to be done however.
As you can also see from the graph above, the next biggest concerns for our community, are anxieties around managing symptoms and managing treatment. For those who may have had a long battle to get a diagnosis, they now face a lifetime of tests, scans and possible treatments. Again, with Rareminds, we developed a leaflet about Living with Uncertainty alongside our disease-specific booklets to help with this.
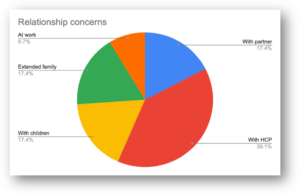
Anxieties around prognosis (38.4%) and treatment/recovery (26.1%) are by far the greatest reason for accessing counselling. However, relationship issues are also impacted negatively, particularly those with health professionals (40%), and thereafter, partners, children and wider family members.
Due to the considerable issues surrounding relationships with health professionals, we developed a leaflet about Working with your Medical Team, which aims to explain what is expected of both health professionals and patients, when working together for the best possible health outcome.
-
-
AMEND’s Member Surveys are distributed every few years, and, although the 2022 survey had a disappointingly low response rate (n=41), it did give us an interesting insight into how our community is coping.
Over half of all those with MEN1, MEN2 and MEN3 responded to say that their condition had negatively impacted on their emotional wellbeing in some way.
This is supported by results from medical studies that show that, in MEN1, fear of disease occurrence, existence of a pituitary tumour, or unemployment are the biggest threats to quality of life. In MEN2, symptoms from metastatic MTC, phaeochromocytomas and hyper- or hypo-parathyroidism have a negative impact.
For all types of MEN, the guilt associated with gene transmission is also a factor. Most studies like these call for care in a multidisciplinary setting where psychological services are available alongside the expertise to recognise patients who are struggling with day-to-day life.
-

-
In MEN3 (MEN2B), there are other, non-endocrine, concerns too. Alongside a big study from Professor Castinetti et al, two smaller studies that AMEND was involved in with MSc students at Queen Mary University London, highlighted the impact on quality of life in those with MEN3 of gastrointestinal and musculoskeletal issues. This extremely rare disease community need a wider inter-disciplinary medical team managed by a key worker to help patients avoid getting lost in multiple specialty appointments. Teams that include MEN3 gastrointestinal and musculoskeletal specialists are extremely rare (if indeed they exist at all at present).
Nevertheless, it’s not all bad news!
Results from our 2022 Member Survey show that most people are happy with their current specialists:
I feel confident discussing my condition with my specialist doctor
MEN1 = 93%
MEN2 = 86%
MEN3 = 75%Issues still remain, however, when we speak with our GPs:
My GP [family doctor] does not understand my condition
MEN1 = 57%
MEN2 = 100%
MEN3 = 50%Although we probably shouldn’t expect our GPs to be well versed in the language of multiple endocrine neoplasia (one of the ‘chicken-and-egg’ reasons why diagnosis times are so bad), it would be good to see more GPs take an interest in MEN when a diagnosed patient is held within their practice.
The good news continues, however. The large European survey looking at Quality of Care for MEN patients, showed that a majority of those who responded were happy with their current care:
Perception of Quality of Care
Good = 43%
MEN1 = 46%
MEN2 = 30%
MEN3 = 50%
Excellent = 36%
MEN1 = 25%
MEN2 = 40%
MEN3 = 44%Respondents also stated that, overall they felt that:
- They were listened to by their HCP
- They had enough time to talk with their HCP
- They were involved in decisions about their care
- Their medical team was knowledgeable about MEN
- They could trust their medical team
This just goes to show how important it is to get to the right place (Centre of Expertise) and see the right specialists.
So, in summary:
- Time to diagnosis and diagnosis itself, alongside symptoms, treatments and concerns about inheritance are all major factors that negatively impact on many patients with any MEN syndrome
- The impact of all these aspects of an MEN syndrome on emotional wellbeing can be significant and must not be underestimated
- Most MEN patients in Europe are happy with their quality of care from specialists, mainly endocrinologists
- General practitioners / family doctors are not knowledgeable about MEN syndromes and this impacts:
- Diagnosis of index case patients
- Routine care of patients outside the specialist centre
In conclusion, patients need:
- To be routinely cared for in accredited Centres of Expertise for MEN with access to interdisciplinary expertise (e.g., musculoskeletal, gastrointestinal)
- Access to emotional support from the point of diagnosis and throughout their patient journey
- The endocrine community and societies to work with primary healthcare professionals and societies to improve time to diagnosis (and therefore prognosis), especially in index cases
- Patient Groups can be a great ally in supporting these patients!